We find a lot of people reporting to into the clinic with upper limb or neck pain that they attribute to spending the majority of their day sat working at a desk or laptop. In our clinic we see increases in this during other periods that are associated with increased desk time e.g. exam revision times, end of year deadlines.
Signs of work related musculoskeletal pain:
- Pain that only occurs when at work e.g. after sitting at for long periods, working at a laptop or computer,
- Pain that settles during holiday periods or change in routine
- Pain that increases with an increase in work volume e.g. deadlines, exam periods
How can you minimise the occurrence of desk related pain?
Whilst your desk set up and posture are important in minimising pain, the reality is that if you sit in any position for a long period of time- no matter what your posture is like, or how high the monitor is, you are going to develop discomfort and potentially pain. That is not to say that optimal desk, monitor and keyboard set up isn’t important- they are a good starting point for optimising your work station for when you are sat at the desk. However the key is a regular change in position. Ideally a change in position every 20-30mins is beneficial in minimising the development of pain. Ideas to facilitate this are:
- central printers away from your desk
- drink breaks
- standing and walking whilst making phone calls
- going and liaising with colleagues rather than emailing
- desks with variable desk heights (standing desks)
One key driver in minimising desk related pain is the exercising away from work. Research shows that the more active you are away from work the more able you are to tolerate being sat for longer periods. So exercising outside of work is really important. Building this into your day e.g. at lunch times can also facilitate a break from the desk. This can be as simple as a walk at lunchtime or a short exercise class.
So remember the key is movement, move often, exercise regularly and you will help minimise your chances of developing desk related pain.

 So we are fully into marathon season so with many races on the horizon for the running community I thought I would discuss the value and art of tapering for race day.
So we are fully into marathon season so with many races on the horizon for the running community I thought I would discuss the value and art of tapering for race day.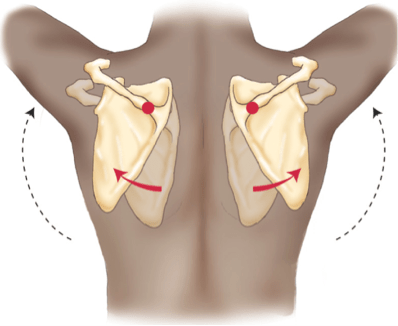 You can try this now, simply try and hold your shoulder blades together and raise your arms, then do the same while relaxed and letting your shoulder blades move. Which is easier?
You can try this now, simply try and hold your shoulder blades together and raise your arms, then do the same while relaxed and letting your shoulder blades move. Which is easier?